Abstract
Introduction: Inhibitor development remains a major complication for patients with hemophilia A. Inhibitors are alloantibodies that neutralize factor (F) VIII activity, which impairs the hemostatic effect of infused FVIII concentrate. Immune tolerance induction (ITI) consists of regular FVIII administration in an attempt to eliminate the presence of inhibitors. There are several ITI protocols with similar success rates around 70%. Still, the ideal ITI regimen and the factors that can influence its success are not well defined.
Objective: This study aimed to evaluate the predictors factors for ITI response among Brazilian hemophilia A patients with high-responding inhibitors who have undergone ITI protocol for the first time.
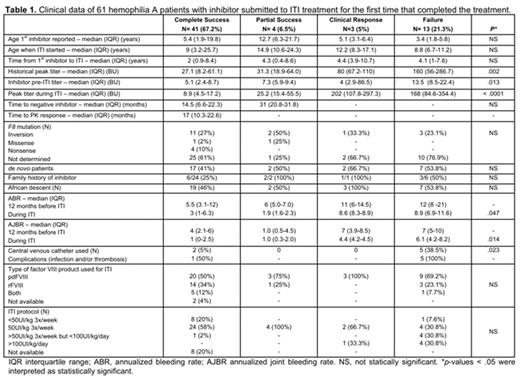
Patients and Methods: We retrospectively analyzed clinical and laboratory data of hemophilia A patients with high-responding inhibitors (peak titer >5 Bethesda Unit (BU) and anamnestic response to FVIII) from eight Brazilian Hemophilia Treatment Centers, who underwent ITI treatment for the first time. ITI outcome was defined as: (i) complete success, negative inhibitor (<0.6 BU) on at least two consecutive measurements, FVIII recovery >66%, and half-life >7 h, with absence of anamnestic response to FVIII; (ii) partial success, negative inhibitor titer and absence of one or two of the PK parameters of ITI success (FVIII recovery > 66% or half-life ≥7 h); (iii) clinical response, inhibitor titer <5 BU and/or FVIII recovery <66% and/or FVIII half-life <7 h, with clinical response to FVIII infusions and no increase of inhibitor titer >5 BU; and (iv) failure, lack of criteria for complete or partial success or clinical response within 33 months of treatment. Statistical analysis were carried out using the Kruskal-Wallis H test.
Results: In this study, we accessed data from 88 patients, from which 61 were analyzed for ITI outcome, having achieved ITI complete success or reached 33 months under ITI protocol. Low-dose ITI protocol was initially used for all patients and started with FVIII concentrate 25-50 IU/kg 3x/week, with dose increment to up to 100 IU/kg daily when a minimum of 20% decrease in the inhibitor titer was not achieved in 6 months. 41/61 (67.2%) achieved complete ITI success criteria, in a median period of 17 months (interquartile range (IQR) 10.3-22.6) after starting ITI. 4 (6.5%) remained as partial ITI success over 33 months of treatment. Among the remaining 16 patients, 3 (5%) had clinical response to FVIII concentrate, without requirement of bypassing agents to achieve hemostatic response, and 13 (21.3%) failed ITI treatment. When comparing groups with different outcomes, statistical analysis revealed that the historical peak titer (p= 0.002), inhibitor titer at the moment of ITI protocol started (p= 0.013) and the peak titer during ITI protocol (p< 0.0001) were important predictors factors of ITI success (table 1). Other clinical factors that possibly interfered with ITI outcome were bleeding rates during ITI treatment, both annualized bleeding rate (ABR) (p=0.047) and annualized joint bleeding rate (AJBR) (p=0.014). Although there was no difference in age at ITI onset, a statistically significance was also observed in the difference of central venous catheter use between complete success and failure groups (5% vs 38.5%; p= 0.023). A possible explanation could be the need for a more intense treatment in the failure group, with a higher demand for venous access. However, the higher risk of infection and thrombosis in this group can also result in lower ITI success. In the group with no ITI outcome analyzed (27/88), 10 (11.4%) discontinued ITI treatment for several reasons and at least 4 of them are no longer using bypassing agents. 16 are still under ITI treatment, from which 7 (43.8%) already achieved clinical response to FVIII concentrate.
Conclusion: In this study, we observed a complete ITI success rate of 67.2% among hemophilia A patients with inhibitor submitted to ITI treatment for the first time. In this cohort, inhibitor titer influenced ITI success throughout different treatment phases, such as historical peak, titer before ITI onset and peak during ITI. The frequency of bleeding episodes during ITI and the use of central venous access were also important predictors of ITI success. This knowledge should contribute to the stratification of prognosis and contribute to decision making in clinical care of patients with high-responding inhibitors under ITI treatment.
Ozelo: Pfizer: Consultancy, Research Funding, Speakers Bureau; Roche: Consultancy, Speakers Bureau; Biogen: Consultancy, Research Funding, Speakers Bureau; CSL Behing: Consultancy; Shire: Consultancy, Research Funding, Speakers Bureau; Grifols: Speakers Bureau; Novo Nordisk: Consultancy, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal